Abortions Caused by Bacteria: Brucellosis, Salmonella, Leptospirosis, Vibriosis
Brucellosis
For complete description on Brucellosis click here.
Summary
In some countries Brucellosis has been eradicated or brought under control by a programe of blood testing, slaughter and heifer vaccination. However in most parts of East Africa there has been no control or vaccination and Brucellosis is common in both humans and animals.
Brucellosis in humans resemble Malaria, and is often mistaken as such unless identified through laboratory testing. Cure of Brucellosis in humans is a very long drawn out and expensive administration of antibiotics and much better avoided by controlling the disease in livestock.
In livestock it is not possible to treat Brucellosis. However, some cattle resist infection and a small percentage of infected cows spontaneously recover.
Cattle/sheep/goats/pigs and camels/donkeys become infected by eating the organism from abortion material, genital discharges, or contaminated pasture, food or water. Abortion occurs 2 weeks to 5 months after the initial infection and generally occurs after the 6th month of pregnancy.
Abortion due to Brucella mostly occurs during the last third of pregnancy. In unprotected herds 40% to 80% of pregnant females may abort or give birth to very weak newborns. After abortion animals give no or only little milk.
Brucellosis is often present in the raw milk, which presents a serious risk to human health as this is a dangerous zoonosis. Always boil milk before consumption!
Signs of Brucellosis
- Abortion is the most obvious manifestation. Animals abort from the 7th month onwards.
- Infections may also cause still births or weak calves, retained placentas, and reduced milk yield. Usually general health is not affected in uncomplicated abortions.
- In less acute (insert dictionary) infections, cattle may give birth to a full term but weak calf, or merely show a retained placenta. Cows may become infertile due to chronic (insert dictionary) uterine infection.
- After abortion, the afterbirth doesn't come out (retained placenta). This can further develop to Mmetritis (infection of the uterus), which often causes infertility.
- In bulls, no symptoms may be seen but if they are, they may include inflammation of the testes, lack of sexual activity and possibly infertility.
- Subcutaneous (under the skin) swellings containing infected fluid may appear on the legs of infected cattle and the placenta often has a thickened leathery appearance with some discolouring
Prevention of Brucellosis
A single vaccination of all female animals between 5 and 8 months of age with S19 vaccine will give adequate immunity for the lifetime of the livestock. Adult vaccination should be avoided if possible to allow serum sampling in an outbreak of abortions to be interpreted without the confusion caused by antibodies due to vaccination with the live S19 vaccine.
Salmonella species
For further information on Diarrhea of the young see here
Salmonella can cause disease in livestock and in humans. They cause diarrhoea and death in young suckling animals, but also diarrhoea and abortion in adult animals. In many countries Salmonella dublin is endemic in cattle and is the most common type of Salmonella causing abortions. Many other Salmonella types may be involved in individual cases. Salmonella also cause disease and abortion in sheep, goats and camels. Aborting animals may have fever and diarrhoea or show no symptoms other than abortion.
Salmonella are also very common causes of diarrhoea in young animals and chicken and can even infect eggs. Humans can get food poisoning from handling raw chicken meat and from consuming raw or undercooked eggs.
All types of Salmonella are zoonotic, they can cause infections and food poisoning in humans.
Abortion due to Salmonella may occur at any time, but is seen mostly during the last third of pregnancy (in cattle between 6 and 9 months).
No specific lesions are seen in the placenta or the foetus.
Leptospirosis
This infection is a problem especially in cattle. Up to 30% of a dairy herd may abort during an outbreak of Leptospirosis. The disease is zoonotic. Leptospirosis infections in humans happen when humans come into contact with infected animals, urine, contaminated water, infected carcases or drink infected milk. In humans Leptospirosis varies, it may be mild, severe or even cause death.
Sorurces of infection:
- Rodents act as carriers and are a source of infection
- Watercourses and standing and stagnant water (e.g. on very wet pastures) can become contaminated and be a source of infection.
- Sheep and goats may be "silent" carriers and a potential source of infection for cattle and humans.
- The infection may be transmitted via urine, milk, abortion material and during mating
Leptospira cause abortions in the last third of pregnancy. Outbreaks are more common when the weather is wet and there is standing water that is contaminated with infective organisms.
Symptoms of Leptospirosis
Cattle may abort without symptoms of illness, or may be acutely ill with severe jaundice (yellowing of gums and white of eyes), fever, haemoglobinuria, photosensitzation (for further information on photosenzitation see here), and in some cases even death.
For more information please also see Leptospirosis under zoonotic diseases
The aborted placenta is yellow-brown and swollen
The foetus usually dies 1-2 days before expulsion and so is already decomposed.
Prevention by:
- Where the vaccine is available, vaccination with a multi-valent Leptospirosis vaccine, every 6 months is recommended.
- Avoid or drain pastures with standing water.
- Sources of infection, such as contaminated water and feed should be identified and eliminated
- Rodents and other vermin should be destroyed. It should be noted that cattle may be life-long carriers of leptospirosis and remain a source of infection.
Diagnosis from Laboratory:
Diagnosis of Leptospirosis is very difficult and only performed by specialized labs. Diagnosis can be made from the foetus organs and the mothers? urine and blood.
A combination of very wet pastures, abortions and jaundice in cattle, occasionally also skin problems is suggestive of Leptospirosis. Abundance of rodents in stables/barns/pastures strengthens this suspicion.
Campylobacter (also called Vibriosis)
For further information see under Birth and Reproduction problems
Scientific name: Campylobacter fetus venerealis and Campylobacter fetus fetus
Common names: Bovine campylobacteriosis, Genital vibriosis
This infection is a problem in cattle and sheep. Campylobacter bacteria cause early embryonic death, infertility and occasionally abortion. This is a venereal disease transmitted during mating. Infected bulls are the source of infection and most outbreaks occur after the introduction of an infected bull into a clean herd. Vibriosis is not zoonotic
- Most cases of abortion occur between 4 - 8 months of pregnancy.
- Usually there are no significant findings other than a mild inflammation of the placenta.
- Diagnosis in the lab is very difficult. Bulls penis sheath washing transported to the lab within 6-8 hours are useful for identification of infection.
- Vibriosis in sheep is evidenced by abortions in late pregnancy and stillbirths
Mode of spread
In cattle the disease is transmitted during mating. It is also transmitted by contaminated instruments, bedding or by artificial insemination using contaminated semen. Individual bulls vary in their susceptibility to infection. Some become permanent carriers, while others appear to be resistant to infection. In young bulls, less than 3-4 years of age, infection tends to be temporary, with transmission apparently relying on sexual contact with a non-infected cow within minutes to days of breeding with an infected cow. Spontaneous clearance in these younger bulls does not seem to be related to any immune response and so re-infection can readily occur. Bulls older then 3-4 years are more likely to suffer chronic infections.
Some cows clear the infection rapidly; others carry it for up to or longer than 2 years. Although most of the genital tract may be free of infection, when a cow eventually conceives the vagina may remain chronically infected throughout pregnancy.
Some infected females can maintain pregnancy but abort usually around the fifth month of pregnancy or sometimes earlier. This means that the presence of the disease can go un-noticed without proper herd fertility records. Breeding females eventually eliminate the infection six months after being infected at service and recover completely. They are then immune and can breed normally.
Signs of Vibriosis
Vibriosis affects both breeding males and females but clinical sings of temporary infertility are confined to females. Clinical signs, other than reproductive failure or abortion, are minimal or absent. The infection of females at conception results in infection in the anterior vagina which subsequently spread to the uterus and fallopian tubes. The infection persists for months and causes the developing foetus to die. The embryonic death initiates cyclical activity in the ovary but these cycles are often irregular with prolonged intervals. Observed abortions are uncommon.
Clinical signs in herds for which good records are maintained are soon evident shortly after the introduction of an infected bull. Animals which have been presumed to have been in calf have irregular returns to heat. In more extensive systems using natural service infection may not be suspected until the calving pattern indicates a delay in conception and a reduced calf crop.
Where the disease has been present for some time indications that C. fetus is present may be much less dramatic, with only heifers, calved heifers and a few susceptible cows being affected, as older animals have acquired natural immunity.
Bulls show no symptoms and produce normal semen. In other words they are fertile, mate normally, and provided they do not have to serve too many returning females, active. The females they serve conceive, but they have been infected. Subsequently the foetus dies and they return to service.
The disease in sheep manifests with abortions in late pregnancy and stillbirths. Ewes may develop inflammation of the uterus after expelling the foetus, which is usually rotten, with 40% having orange-yellow spots in the liver. The disease in sheep is acquired by mouth, not via the ram.
Diagnosis
This would be based on the history of late abortions and return to heat after successful mating.
Laboratory diagnosis is based on the vaginal mucus agglutination test. Samples are taken from at least 10% of the herd, concentrating on those females most recently exposed to infection by service, open cows or those returning to their third or fourth service. Tampons are placed in the anterior vagina and sheath washings are taken from suspected bulls.
Diagnosis in sheep depends on finding the organism in the stomach, placenta or uterine discharge.
Prevention
Use of Artificial Insemination with semen from non-infected bulls should eliminate the infection from an infected herd within two complete breeding cycles.
Care must be taken when buying breeding bulls. A veterinary certificate stating that they are free of Vibriosis (and Trichomoniasis) should be insisted upon.
Where AI is not feasible, all animals in a herd should be tested and the infected and non-infected animals managed separately. This approach requires a high level of management and careful veterinary supervision.
Vaccination is practiced where the vaccine is available.
In sheep strict hygiene and regular vaccination, where the vaccine is available, should be practiced.
Control is by:
- Vaccination
- Replacing natural mating by artificial insemination until all cows have had two pregnancies.
- The infected bull may be treated with Streptomycin injection combined with oil-based Streptomycin applied locally to the penis is possible. This treatment must be carried out on 3 consecutive days and should be applied by a trained professional. Bulls are of course susceptible to re-infection if they mate with an infected female.
- It is not necessary to treat infected cows, they generally recover spontaneously.
- In sheep the use of tetracyclines may help to prevent exposed ewes from aborting.
Abortions and infertility in cows caused by Vibriosis look exactly as those due to Trichomonas (see under Trichomonas).
Abortions Caused by Bacteria: Listeriosis, EAE, Q-Fever
Listeriosis
Listeriosis is a zoonosis and may spread to people via raw milk, it can cause severe infections that can sometimes lead to death.
The organism Listeria is widespread in the environment being present in the soil, sewage effluent, bedding and feedstuffs (especially poor quality silage). Cattle, sheep and goats get the disease by eating infected feedstuff. Sheep and goat are more susceptible to Listeriosis than cattle. The infection then travels to the placenta, causing inflammation.
Many outbreaks are associated with the feeding of poor quality silage, especially if the silage contains soil.
Signs of Listeriosis:
- Central nervous symptoms (Encephalitis, e.g. one ear hanging down) and sometimes eye infections.
- Sporadic abortion, the foetus is usually decomposed when aborted.
- The placenta is inflamed with multiple, yellow or gray coloured spots in the cotyledons; similar spots are found in the liver of the aborted foetus.
Abortion usually occurs in late gestation and is usually sporadic, although rarely abortion storms may occur.
There is no vaccine. Although antibiotics have an effect on Listeria, the cure rate after injecting antibiotics is very poor. Animals that do recover and return to feeding often still show some nervous symptoms. Control should involve an awareness of the risks of feeding poor quality silage contaminated by soil.
Enzootic Abortion of Ewes (EAE)
This disease can be a big problem in sheep and goats. It is caused by a bacterium called Chlamydia (old name) or Chlamydophila (new name), which can cause sporadic abortion in cattle and also infects people.
Infection is via feeding in a contaminated environment. During the next pregnancy the organism invades the placenta and causes abortion.
If rams are infected, they may develop inflammation of the testicles and the organism is excreted in the semen, but spread by the ram does not play a role.
Signs of Enzooic Abortion
Abortion storms, involving up to 30% of ewes in a flock, are a feature of EAE, especially in intensively managed flocks. Ewes are not noticeably ill. They abort only once from EAE and have solid immunity after the abortion.
Abortions occur in the last three weeks of pregnancy and weak, live lambs may be born alongside dead lambs.
The placenta between the cotyledons is thickened with a brownish colour over the surface. The foetuses are usually fresh.
The organism is present in large numbers in the abortion products and vaginal fluids for up to three weeks after the abortion, leading to heavy contamination of the environment and infection of other sheep. Some ewes can become permanent carriers of the infection.
Diagnosis
Examination of fresh placenta is the method of choice for the diagnosis of EAE, but make sure to use gloves!! Alternatively, vaginal swabs or swabs taken from the coat of aborted foetuses can be used.
Prevention and Control
Various vaccines are available, including an inactivated vaccine for use in pregnant animals, but they are not marketed in Kenya / East Africa.
In the face of an outbreak, mark and isolate aborting ewes, dispose of bedding and abortion products and disinfect pens. Ewes that have aborted should not be used to foster lambs.
| WARNING: Pregnant women should NOT deal with lambing ewes and goats or any aborted material from sheep and goats. Many infections, which cause abortion in sheep and goats, are transmissible to humans. Especially the agent of EAE( Chlamydophila) is capable of causing severe disease and abortion in pregnant women. - Toxoplasma, Q-Fever, Salmonella, Leptospira and Listeria can also cause disease and abortion in humans |
Q-Fever Coxiella burnetii
Q-Fever was first identified in Queensland, Australia; hence its name.
This is a bacterial disease, and an important zoonosis (an animal disease that can be transmitted to humans). Q-Fever is caused by an organism called Coxiella burnetii. It is found all over the world, in every country where it has been sought.
Its main importance is its ability to infect man, and to cause a severe respiratory disease. In ruminant livestock Q-Fever leads to abortions, inflammation of the lining of the uterus and mastitis.
Q-Fever is a disease passed to humans from sheep. People working around domestic sheep should consider getting vaccinated against this disease. The disease can be acquired from the inhalation of aerosolized barnyard dust should it contain infected dried urine, manure particles, or dried fluids from the birth of calves, or lambs, or raw milk.
Coxiella burnetii is an extremely difficult organism to eliminate. It is very tough, resisting most disinfectants, heat and drying, and surviving for years in dust.
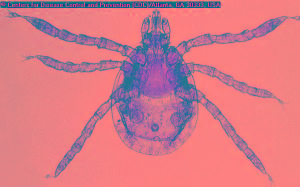 |
| View of a larval Ixodide, Dermacentor marginatus[I/] hard tick. This tick species is known to be a vector for Q-fever, which is caused by the bacteria Coxiella burnetii[I/]. |
|
© Picture from CDC/Donated by the World Health Organization, Geneva, Switzerland
|
Mode of spread
There are two different cycles:
1. The bacterium cycles between small free-living ground mammals and ticks
2. The bacterium cycles in domestic ruminants (cattle, sheep, goats), independent of the wild animal cycle , ruminants infect each other via abortion fluids and abortion materials that contaminate stables and pastures
Ticks can act as reservoirs of the Q-Fever organism. Tick-free cycles in domestic ruminants allow the organism to be concentrated in the genital tract and udder, from where large numbers are shed in milk, faeces or urine, or, from the genital tract at lambing or calving.
A wide variety of other animals and birds may also be infected and play a part in spreading Coxiella burnetii. These include dogs and several species of birds.
At-risk animals, and man, become infected by inhaling infected fluid discharges in the air or dust loaded with dried discharges.
The disease is highly infectious. Animal handlers are particularly at risk from infection, especially at lambing or calving, from inhalation, ingestion or direct contact with birth fluids or afterbirth.
However the main route of most human infections is by inhalation of contaminated air droplets or dust originating in infected ruminants or other animals e.g. cats.
Spread can occur up to 10 kilometres from the source of infection by wind dispersal of dried reproductive products, such as afterbirth, genital discharges, etc. from infected sheep, cattle and goats, depending on wind condition.
Symptoms of Q Fever
Infection in ruminants is usually symptom-free, but it can cause late abortions, inflammation of the uterus and mastitis in sheep and goats, together with loss of appetite, and offspring of carrier animals can often appear weak, showing low vitality. Large numbers of organisms are shed in the milk, urine, faeces, saliva and especially through the afterbirth and uterine discharges. These are the main sources of infection for man. Cows may shed the organism in milk for years.
Symptoms of Q- Fever in man can easily be mistaken for those of flu: fever, headache, chills, muscle pains, lack of appetite and nausea. The incubation period is about 2 to 3 weeks, and the disease lasts for 1-2 weeks.
In severe and chronic cases, pneumonia, hepatitis and endocarditis may occur and in some cases the infection causes death, as has happened in the recent outbreak in north-west Europe.
The infection of pregnant women can result in abortion or premature delivery.
The main route of infection is by inhalation of infected dust or aerosol droplets. Drinking contaminated raw milk products in unlikely to cause any symptoms of disease.
Diagnosis
There are no clinical signs in domesticated animals. The sudden appearance of an influenza-like disease in man following an association with cattle, sheep or goats, or with their carcases, hides, tissues, or following an autopsy, should be regarded as evidence of infection.
But neither the history nor the clinical picture is enough to prove the presence of Q Fever. A definite diagnosis can be established only by lab tests to identify the bacteria that causes the disease in the blood or sputum of a patient.
Other causes of abortion in ruminants should be considered when reaching a diagnosis.
Control
Recovered animals remain infected and infective for many years and sometimes for life. It is therefore necessary to take steps to limit the spread of infection by adopting hygienic precautions at the time of lambing, kidding and calving. In particular afterbirths should be destroyed. In known infected flocks or herds pregnant animals should be separated from others indoors.
Vaccines are available and are being developed in Europe and when given to uninfected animals have prevented infection. When given to previously infected animals the vaccines have improved fertility and reduced the shedding of organisms.
This disease is probably much more common than is realized, due to under reporting and lack of facilities in reaching a diagnosis.
Treatment
In animals this is seldom attempted. Oral tetracyclines (antibiotics) are reported to have a beneficial effect, but their use carries risks in ruminating animals such as cows, and is therefore not recommended.
