Introduction
This chapter contains information about twelve zoonoses we have selected, because: they may cause serious illness in people; they are very common; or there has been a lot of attention surrounding this disease recently or in the past. In the text, we have tried to provide information on the incidence of the specific zoonoses: in which regions they occur and how often. Because exact data on the occurrence of these diseases is difficult to provide for every region, we advise you to contact your local veterinary service.
Zoonoses highlighted in this Chapter
- Anthrax
- Avian Influenza
- Bovine tuberculosis
- Brucellosis
- Cysticercosis
- Chagas' disease
- Echinococcosis
- Influenza: see avian influenza
- Leptospirosis
- Rabies
- Sleeping sickness
- Tapeworms: see Echinococcosis or Cysticercosis
- Toxoplasmosis
- Trypanosomiasis: see sleeping sickness
- Tuberculosis: see bovine tuberculosis
- Viral Hemorrhagic Fevers
- Yellow Fever
Anthrax
|
Anthrax is also called carbúnco or splenic fever. It used to be a global disease, but many countries have succeeded in eradicating it. The disease is prevalent in East Asia, West and Central Africa, Madagascar and Central America. And, due to breakdown of veterinary services, the incidence of anthrax is increasing again worldwide, for example in Eastern Europe.
Transmission and symptoms in humans
There are three forms affecting humans: 1.) The cutaneous form or skin form is the commonest form and is transmitted via the skin by touch from the carcass, blood, wool, bones or skin of an animal that died of anthrax. It causes vesicles in the skin that are only slightly painful and black in colour. Without treatment, one out of five infected people die. 2.) The respiratory form is caused by inhalation when working with leathers and wools in a closed atmosphere. At the onset it seems like a common respiratory infection, but days later it becomes more serious and may even cause death. 3.) The intestinal form can be contracted from eating the meat or drinking the blood of an animal affected by this disease. The symptoms of the disease are violent, expressed by vomiting and bloody diarrhoea. Some 25 to 75 % of the patients die.
|
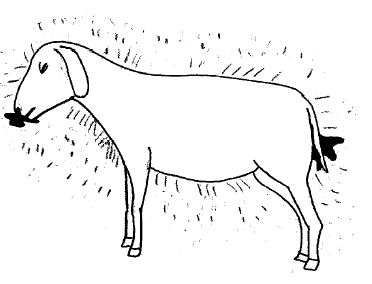 |
| Animal that died from anthrax with black blood from nose, mouth, vulva and anus |
|
© Agromisa Foundation and CTA, Wageningen, 2008
|
Symptoms in animals
Anthrax can affect all animals, domestic and wild. Animals become infected when they drink contaminated water or eat contaminated grass from a spot near where a carcass with anthrax lies exposed. In animals we can also see three forms:
1.) The peracute form progresses rapidly! The owner mostly only finds a dead animal and suspects that it died from poisoning or lightning. As the blood does not coagulate normally, it is possible that the blood in and around the nose, mouth, vulva and anus is black in colour. The carcass does not become rigid.
2.) The acute and sub-acute form exhibits the following symptoms: fever, nervousness, difficulties with breathing and walking, convulsions (fits) and death. The blood is not always observed to be black.
3.) The chronic form develops somewhat slower, with a swollen tongue and bloody foam from the mouth, but the animal soon dies because it cannot breathe.
Prevention
- Any animal that dies suddenly is suspicious of being infected with anthrax: do not do an autopsy on an animal that has died suspiciously or has blood oozing out of its natural openings (it can be dangerous)!!
- Avoid letting wild dogs and animals open the carcass;
- Destroy the carcass as rapidly as possible (by burning or to burying with caustic lime).
- Do not eat meat or blood from an animal that died of an unknown disease.
- Be aware of small skin injuries and take care of personal hygiene.
- Ventilate and use proper working clothes in places where products of animal origin are handled, especially leathers and wool.
- Groups of people, who by their work are at serious risk, can be vaccinated.
- Vaccinate cattle and goats annually in regions where anthrax is common.
Avian Influenza
Avian or bird influenza is a disease that mainly affects poultry. Wild birds can also be infected but normally have no symptoms. Avian influenza can also affect humans, pigs, horses and many other animals. Although all influenzas are related, the type of influenza that infects one animal species usually does not affect another animal species. However, there are exceptions.
|
When humans get infected with avian influenza the symptoms are red eyes and those accompanying a (common) flu-like illness, which is mostly very mild. In chickens, one of the alarming symptoms is the sudden death of many chickens in a short space of time. But the disease may also occur without causing symptoms, or with only fatigue, diarrhoea and respiratory problems. A certain type of influenza, called H5:N1, is the cause of the current avian influenza-epidemic. This type can also cause severe pneumonia in humans, which luckily seldom happens. However, there is a very real chance that people who get the disease will die.
|
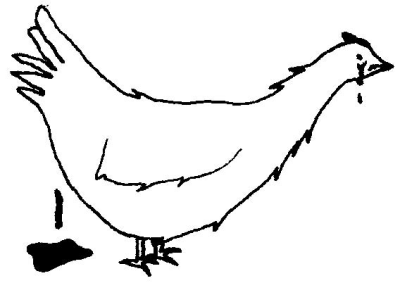 |
| Chicken with symptoms of avian flu. The chicken has diarrhoea and runny eyes. |
|
© Agromisa Foundation and CTA, Wageningen, 2008
|
Transmission: how do people get this disease?
Transmission occurs via direct contact with live and dead birds that have been infected, especially wild water birds and poultry. Humans can get infected through contact with the faeces and blood of infected birds.
Prevention
Do not touch birds if there is a hint of suspicion of avian influenza, for example, when you find many dead birds together. By touching these animals, you could spread the disease to chickens. Note: avian influenza in poultry cannot be cured. If avian influenza is alerted in your region, keep your poultry inside and make sure that they cannot come into contact with wild birds and other poultry.
Vaccination against avian influenza in poultry is possible. Ask a veterinarian about this.
Challenges
Why is there so much to-do about avian influenza in humans? At this moment, poultry owners should be aware of the fact that they can get seriously ill from chickens with avian flu. The main problem is the fear that this influenza virus may mutate (change) and then become extremely dangerous to people. Authorities are afraid that such a dangerous influenza could kill millions of people all over the world. On the other hand, there is no real evidence that this will ever happen. We just don't know.
Bovine tuberculosis
There are three types of tuberculosis in humans: human tuberculosis, bovine tuberculosis and avian/porcine tuberculosis. Most cases of tuberculosis in humans are human tuberculosis and this is not a zoonosis. The other two are zoonoses, of which bovine tuberculosis is the most significant.
Symptoms in humans
Bovine tuberculosis most often affects weak or debilitated people. Thus, patients with immunodeficiency (for example patients with AIDS) run a greater risk of contracting the disease. The disease causes abscesses of different sizes that appear in the lungs, which in time can become hardened. Sometimes it can invade other organs of the body. It is a chronic disease. The patient coughs a lot, has pain in the chest, fatigue and sometimes dies. The treatment based on antibiotics is lengthy and expensive.
Transmission: how do people get this disease?
People get bovine tuberculosis through consumption of raw (uncooked) milk and other dairy products made from raw milk. It can sometimes be transmitted through the air (airborne), for example, when humans and cattle live together in the same tent or house.
Symptoms in animals
Mycotuberculosis bovis is a cattle disease. It is a chronic disease of the lungs. Transmission between cows is airborne. Other species, like cats and dogs, can become infected by consuming raw milk, but they have natural resistance and do not transmit the disease to people.
Prevention
- Boil all milk before consumption.
- Vaccinate newborn children with tuberculin vaccine.
- Meat inspection and inspection of carcasses: cows with tuberculosis have tubercles (small bumps) in their lungs, intestines and other body parts.
- People with a chronic cough should be referred to a medical centre for tuberculin testing, X-rays and, if necessary, proper treatment.
- Test cattle with the tuberculin test and if the test says that the animals are infected with tuberculosis, kill these animals. In some countries there is a certificate-system where tuberculosis-free herds get a certificate. It is then necessary to prevent people with tuberculosis from working with cows, because through them the cattle can become sensitized to the tuberculin test.
Brucellosis
Brucellosis, a disease that has spread worldwide, has different names: infectious abortion and Bang disease in animals; and undulant fever or Malta fever in humans.
Brucellosis in humansPeople get brucellosis through direct contact with ill animals and by touching aborted foetuses, placentas, secretions, birth channels and excrements. Brucellosis can also be contracted from drinking uncooked milk or eating cheese made from raw milk. |
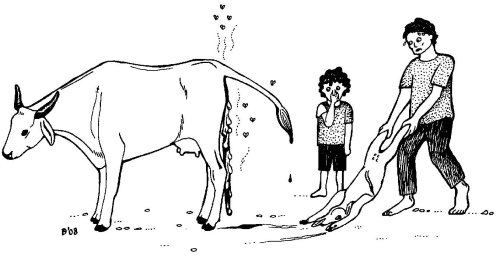 |
| Cow showing a stillborn foetus and placenta. |
|
© Agromisa Foundation and CTA, Wageningen, 2008
|
Some persons infected with the Brucella bacteria do not have any symptoms at all. Sometimes you will see acute fever, chills, insomnia, sexual impotence, generalized constipation, pains and sometimes nervousness and depression. These symptoms are easily confused with the symptoms of malaria, and therefore people may not think that raw milk has made them ill. In humans brucellosis can also cause abortion!
Brucellosis in animals
Animals can become infected when they lick or eat the foetus, placenta or liquids from an animal that has aborted, and from eating the hay where a dead foetus had lain. A female animal can also get brucellosis when she mates with a male animal that is infected. Brucellosis can be even be transmitted via artificial insemination.
The main symptom in all animals is abortion, often combined with retention of the placenta, a lower milk production, mastitis and infertility:
- In cattle, abortion occurs from the 5th month of gestation.
- In goats and ewes the main symptom is abortion in the 3rd or 4th month.
- In pigs, abortions occur in the second half of gestation. Besides abortion, brucellosis may also cause abscesses in pigs.
- In horses and dogs, abortion is rare. Cats are resistant to brucellosis.
Prevention
- Boil milk before drinking it. Some people say that acidity also kills the brucellosis bacterium, but this is not certain.
- Veterinarians, cattle dealers and slaughterhouse workers should use protective clothing (mainly gloves) and have regular medical checkups. Vaccines exist for people who are at high risk.
- In case of an abortion: separate the animal, bury the foetus and placenta and burn the grass/straw where the animal has aborted.
- Vaccination of young female animals is recommended if there is much brucellosis around. Contact your veterinary services for vaccination. There is no vaccine for pigs.
- In countries where brucellosis is not common, control of the disease is done by testing cattle and eliminating cattle with positive test results.
Chagas' disease
|
Chagas' disease, or American Trypanosomiasis is only seen in the Americas. The symptoms it causes are slightly different to those of African sleeping sickness and it is easier to cure. Prevention of American and African trypanosomiasis is the same. Chagas' disease is transmitted to humans by an insect (beetle-like) that is 2 centimetres in length called Triatomíneo, better known as "vinchuca". Symptoms in humansChagas' disease is a chronic disease caused by the bite of the vinchuca and it can take years before symptoms appear. The disease starts with fever or other non-specific signs. Specific is the Romaña's sign: oedema (swelling) of the eyelids and eye infections. Heart problems can also occur.
Extra PreventionClean the cages of chickens and guinea pigs every week and try to get rid of the insects using smoke. A person bitten by a vinchuca should go to a doctor to have a blood check. There are special medicines to completely eliminate the parasite, but only shortly after the bite. |
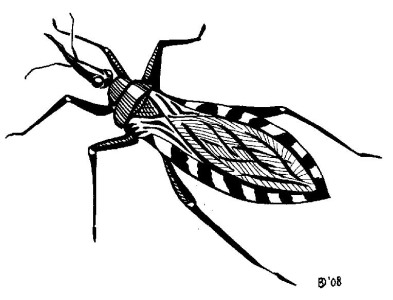 |
| The vinchuca |
|
© Agromisa Foundation and CTA, Wageningen, 2008
|
Corona
Tapeworms and Cysticercosis
|
Tapeworms live in intestines of humans and animals and can measure up to 10 metres! Tapeworms are made up of a lot of small segments, called proglottids. These segments become detached and are excreted with the faeces. They look like rice grains. Each segment contains more than 10,000 eggs. If humans or animals ingest those eggs, the eggs hatch and the young worms migrate through the body (especially the muscles) of the animal or human. They form cysts in muscles and organs. If you have tapeworms in your intestines, it is called taeniasis; if you have cysts, then it is called cysticercosis. |
 |
|
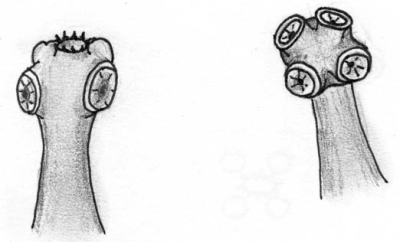
Left: the head of Taenia solium , the pig tapeworm, under a microscope. |
|
Right: the head of Taenia saginata, the bovine tapeworm, under a microscope. Both heads are enlarged approximately 100 times. © Agromisa Foundation and CTA, Wageningen, 2008
|
The three types of tapeworms of significance to humans are:
1.) The pig tapeworm (is called Taenia solium): this is a tapeworm in humans and forms cysts in pigs and in humans
2.) The bovine tapeworm (is called Taenia saginata): this is a tapeworm in humans and forms cysts only in cattle
3.) The fox tapeworm and the dog tapeworm both cause echinococcosis.
Porcine cysticercosis poses a serious problem to public health in regions where pigs are kept in the same place as where people defecate.
This is especially so where there are no latrines and where there are open rubbish dumps. In Latin America, the pig tapeworm is also called "triquiná". But this is in fact the real name of a totally different zoonotic worm (Trichinella). Switching of names makes prevention more difficult, because you are never really sure what people mean.
Symptoms in cattle and pigs
Generally, there are no clinical symptoms in cattle or in pigs. Cows can get infected by eating grass that contains tapeworm eggs. This has to do with the people who defecate in open fields. Pigs get mostly infected when they directly eat human excreta. There are no medicines that can kill the cysts in the cow or pig. The cysts in pigs can sometimes be detected when they are alive, by inspection of the tongue. The cysts are white, round vesicles measuring between 0.5 to 1 centimetre in diameter.
Transmission: how do people get this disease?
The growth and reproduction cycle of tapeworms is as follows:
- Once in the human intestines, the adult tapeworm lays eggs there.
- The eggs are expelled with the faeces and are eaten by cattle or pigs.
- The eggs hatch in the cow or pig.
- The larvae (from the eggs) grow and form cysts (vesicles or round holes) in the muscles.
- When humans eat raw or badly cooked meat (= muscles), the larvae wake up and grow into adult worms again.
So, the tapeworms need the animals to hatch from the eggs and to grow. This cycle sometimes goes wrong in the case of pig tapeworms, when the larvae eaten by humans get confused and migrate through the human body to form cysts in different parts. It can happen that they form cysts in the human brain or liver.
Symptoms in humans caused by the tapeworms
The symptoms of tapeworms are less serious than the symptoms caused by the cysticercus; only sometimes causing stomach aches, diarrhoea, poor appetite and malaise.
Symptoms in humans caused by cysticercosis
The pig tapeworm is the tapeworm that causes cysticercosis in humans. Cysts can be present in all parts of the body. These cysts may become so large that in the end they will become life threatening, but mostly this will not happen. Cysticercus in muscles does not display many clinical symptoms, but when cysts grow in the brain you can get neurocysticercosis. Then the symptoms are severe headaches and epilepsy.
Prevention
The main problem is cysticercosis, caused by the pig tapeworm. To prevent cysticercosis, it is important to interrupt the infectious cycle between humans and pigs.
- Educate people about cysticercosis and the lifecycle of the tapeworm. People must be made aware of the fact that if they defecate in a place where pigs can come, they contribute to the infection of other people.
- Promote the use of latrines.
- Wash hands after defecating and before cooking or eating. This aspect is especially important for children.
- When there are white pieces like grains of rice in the faeces, an antiparasiticum must be administered to all members of the family.
- Cook pig meat very well.
- Inspection of pig meat. The traditional control in markets and fairs is insufficient; more and better control is needed.
- Keep pigs in a stable.
These measures also prevent taeniasis from cattle: use latrines, keep animals in a stable or a field with a fence around it and observe strict meat control (of pork and beef) in slaughterhouses.
Do not buy meat if you are not sure whether is free from cysts!
Taenia solium ,Taenia saginata
- Lifecycle in humans and pigs
- Forms cysts in pigs and humans
- Proglottids are not active: they are passively excreted with the faeces
- Pig cysticercosis is dangerous!
Taenia saginata
- Lifecycle in humans and cattle
- Forms cysts in cattle
- Proglottids are active: they creep out of the anus, also without faeces
- Cattle tapeworms are annoying, but not dangerous
Echinococcosis
Echinococcosis is caused by tapeworms from foxes, wolfs and dogs. It is also called hydatidosis. The disease is present globally and is especially a problem in rural communities.
How do people get the disease
These tapeworms live in the intestines of dog-like animals. They produce eggs that are excreted with the faeces. When a susceptible animal (cattle, sheep, pigs, mice, humans) accidentally ingests the eggs, the eggs will hatch in the intestines of the animal or person. After hatching, the larvae can move to different organs where they will start to grow as cysts (hydatids). When a carnivore eats the infected animal, the larvae develop into adult tapeworms in the intestines of the carnivore.
Symptoms in humans
The adult parasites do not cause disease. The larva, however, can be dangerous. Symptoms depend on where the cyst is, often in the liver and/or lungs. Cysts grow slowly and may not show any signs for up to 20 years before becoming large enough to be visible as an abdominal swelling, or starting to cause problems by pushing on different organs. Death often occurs from this extreme compression of vital organs. Symptoms of liver cysts can include jaundice, abdominal pain and vomiting. Pulmonary cysts give rise to respiratory problems. Brain cysts may cause headaches and seizures (fits). The only curative treatment of cysts is surgical removal, but this is not always possible.
Prevention
Eradication of this disease is very difficult and very costly. A rich country like Australia, for example, tried for ten years to get rid of echinococcosis but failed, because wildlife (dingoes, small rabbits and rodents) is a reservoir for echinococcosis. People have to prevent the disease from occurring by paying attention to the following:
- Routine deworming of domestic dogs and cats
- Not giving the remains of sheep and cattle to domestic animals
- Not allowing animals in the slaughterhouse other than those for slaughter
- Preventing domestic animals from wandering and straying
- Handling wild carnivores with care and always washing hands after handling
- Carefully washing or cooking before eating all wild fruits or vegetables picked directly from the ground.
There are no vaccines.
Leptospirosis
|
Leptospirosis is a zoonosis that lurks in water, soil and foods contaminated by urine of infected animals, especially cattle, rats and pigs. Other names for leptospirosis are: fever of the rice fields, fever of the cane plantations, enfermedad de los porqueros (Spanish) and Weil's disease. The disease can become especially problematic after heavy floods. In the past, this was what happened in parts of Ecuador, Cuba and Nicaragua where many cases of leptospirosis occurred after floods.
Symptoms in animalsThe disease mainly affects cattle, dogs, rats and mice, and has a wide range of symptoms, though in some cases no symptoms at all. In cows it can cause mastitis, abortion, infertility and bloody urine. Dogs can become seriously ill with fever and infected kidneys. |
 |
|
People drinking water from a source that may contain leptospira from the urine of rats run the risk of getting seriously ill |
|
© Agromisa Foundation and CTA, Wageningen, 2008
|
Symptoms in humans
The symptoms vary much and can even be absent. In general two clinical types are distinguishable:
1.) Icteric leptospirosis, the more serious of the two: produces fevers, flu-like symptoms and yellowish skin. The kidneys can fail.
2.) Anicteric leptospirosis is less severe, though people can die of it! The symptoms are similar to influenza. The patient usually recovers in a month. This form is the commonest.
Prevention
- Avoid contact with the urine of animals.
- Pay attention to personal hygiene and use a separate set of clothes when working with animals.
- The leptospira bacteria that cause leptospirosis will die in the sun, so you can hang out your working clothes in the sun for a day.
- Drain low land as best as possible.
- Control rats and mice.
- Avoid swimming, bathing or washing in fresh water that might be contaminated by the urine of animals.
- Appropriate vaccination for pigs, cattle and dogs.
Rabies
Rabies, or rage, is one of the most important and dangerous zoonoses! It is present in almost all countries over the world and as much in the cities as in rural areas.
Transmission: how do animals and people get infected?
Rabies is transmitted by the bite of a rabid animal, mostly a dog. Be especially aware of stray dogs! In rural parts of Latin America, vampire bats are dangerous as they are also able to transmit rabies. In some countries, especially in Africa, jackals, mongoose and other wild animals can transmit the disease; skunks and raccoons in the USA.
Symptoms in humans and animals
The symptoms are more or less the same in both humans and animals. They may occur after 10 days, but it can also take up to 10 months to appear, depending on the location of the bite. If the bite was near the head, this period will be closer to ten days, whereas if the bite was in a foot, for example, it could take longer.
The first symptoms are anxiety and pain around the bite wound. People also mention headache. Soon the person will not be able to tolerate light and sound and will start salivating profusely. The disease will cause spasms, paralysis and difficulties with swallowing, which is why the disease is also called "water fear" as the person - although very thirsty - is unable to drink.
In animals, the symptoms are more or less the same. Dogs and cats exhibit "furious rabies": the animals have the same symptoms as mentioned above, but also become nervous, excited and aggressive. Ruminants and horses exhibit a more quiet form, "dumb rabies": the animals become very timid and shy and not excitable at all. The dumb form can also affect dogs, which is then extra dangerous because people do not recognize it as rabies.
Once a person or animal has symptoms, there is no treatment and the only outcome is death!
Prevention
- Do not touch any animal with nervous symptoms and changes of character, and do not pick up a fallen vampire bat.
- After a bite:
1.) Catch and lock up the dog.
2.) Wash the person's wound with abundant water and soap!
3.) Go to a health centre to start anti-rabies vaccine treatment. If the dog responsible for the bite remains healthy for the duration of 5 days after the bite, the treatment can be stopped.
Some countries have an eradication programme, meaning vaccination programmes for humans and animals, and birth control for stray dogs. In countries where vampire bats play a role, a monitoring system can be set up to control rabies in these bats.
Sleeping sickness
Sleeping sickness or African trypanosomiasis is a disease that affects humans. Wild and domestic animals (particularly antelopes, buffalo and cattle) can also be infected with a subspecies, but they do not get symptoms. Sleeping sickness only occurs in sub-Saharan Africa. Another human form of trypanosomiasis occurs in the Americas and is known as Chagas' disease (see earlier chapter).
How do people get Sleeping sickness?
The disease is transmitted by the tsetse fly.
Symptoms in humans
First there is redness, pain, and swelling at the site of the fly bite, but this is often ignored. The disease starts with fever, weakness, headaches, joint pain and itching. A characteristic symptom is a nut-sized bump in the neck, behind and below the ear (Winterbottom's sign). In a later phase, involvement of the brain produces the more characteristic signs of the disease: confusion and unpredictable mood changes. The person is unable to sleep at night and fall asleep during daytime, which gives the disease its name. Without treatment, the disease is fatal.
There are two forms of sleeping sickness:
1.) In central and western Africa (Gambian form), where the first phase can last for months or years without any manifestation of symptoms, suddenly starting in the second phase.
2.) In southern and eastern Africa (Rhodesian form), where the illness develops in a few weeks and the two phases are evident.
Prevention
Avoid contact with the tsetse fly:
- Wear thick protective clothing. Tsetse can be quite aggressive and bite through thin fabrics.
- Wear khaki or olive coloured clothing, because tsetse is attracted to bright and very dark colours.
- Use mosquito nets.
- Avoid places where the tsetse lives (vegetation along watercourses extending to vast areas of wooded savannah).
- Try to improve the construction of the houses: preferably plaster walls and ceilings and do not use hollow canes to build a house.
- Repellents do not work on tsetse flies. Medicines that work are hard to come by.
Toxoplasmosis
Toxoplasmosis is a very common parasitic disease both in the western world and in developing countries. A microbe, a protozoan that has a complex life cycle, causes it. Toxoplasmosis is especially dangerous to pregnant women and the foetus.
Transmission: how do people get this disease?
The cat plays a fundamental role in the infectious cycle. Cats become infected with the parasite when they eat wild mice or birds, after which the faeces of the cat will soon contain eggs that are infectious to other animals or humans. Flies, mice and cockroaches can transport the eggs to the kitchen and the rest of the house. Humans get infected most commonly by eating raw or inadequately cooked meat of pigs and sheep that have been in contact with cats.
Symptoms in humans
Toxoplasmosis generally produces no symptoms. Infected humans sometimes have fever, pneumonia, heart problems and brain damage, especially those with a weak immune system. In pregnant women, the infection can affect the eyes and the brain of the foetus. The child can be born with hydrocephalus (commonly known as water on the brain caused by excess fluid in the brain), epilepsy, deafness or can be retarded.
Symptoms in animals
Infected cats, dogs, goats, pigs, horses, cattle, rabbits, guinea pigs and wild animals generally have no symptoms. The infection in sheep, on the other hand, can be the cause of abortion, nervous symptoms and eye problems.
Prevention
- Protect food against flies, cockroaches and mice.
- Wash your hands after handling raw meat and avoid eating raw or insufficiently cooked meat. This is especially important for pregnant women.
- Wash hands after touching soil where cats might have defecated.
Viral Hemorrhagic Fevers
Hemorrhagic fevers are rare but deadly diseases that are caused by a virus. Examples are Crimean-Congo hemorrhagic fever, Ebola hemorrhagic fever, Marburg hemorrhagic fever, Rift Valley fever, Nipah fever, Yellow fever and Lassa fever. Yellow fever is further explained in next the chapter Yellow Fever.
How do people get these diseases?
Mosquitoes or ticks transmit most hemorrhagic fevers. Nipah fever is transmitted by bats and pigs; Lassa fever by rodents. Ebola and Marburg can also spread from person to person (but are extremely rare diseases).
Symptoms in humans
Fever and bleeding are the symptoms in humans and is the reason why they are called hemorrhagic fevers. Most patients die from shock, coma, seizures and sometimes kidney failure.
Prevention
There is no cure for these diseases, so prevention is important. Vaccines exist only for yellow fever. For the other diseases, control of rodents, ticks and mosquitoes is vitally important. Clear away rodent nests and make sure that they cannot enter your house. Use insect repellents, mosquito nets, window screens and wear clothing that covers arms and legs
Yellow Fever
Yellow fever is a disease that affects monkeys and humans, called "black vomit" in some areas. The disease is found in tropical areas of South America and Africa. There is no explanation as to why the disease does not occur in tropical Asia, despite favourable conditions. Transmission of yellow fever occurs mainly during the rainy season, in moist savannah zones.
How do people get yellow fever?
Yellow fever is transmitted to humans and monkeys by the bite of infected mosquitoes. These mosquitoes are different from those carrying malaria and, most important of all, they are daytime biters. So general precautions to avoid mosquito bites should be followed. These include wearing light-coloured clothing with full-length trousers and long sleeves, using insect repellent on exposed skin and mosquito nets.
Symptoms in humans and animals (monkeys)
Symptoms can appear 3-6 days after infection. They include fever, headache, muscle pain, loss of appetite, abdominal pain and jaundice. After 3-4 days, the general condition normally improves and most individuals will recover. But in some cases a high fever returns within 24 hours when the infection has taken a turn for the worse. If this happens, the sick person becomes very tired and bleeding from the mouth and nose can occur. It is difficult to distinguish from other diseases, especially in the early stages of the disease. The symptoms in monkeys are the same as in humans.
Prevention
Vaccination is the single most important measure for preventing yellow fever. But there are also groups of people who cannot be vaccinated, because it would be too dangerous. They are: infants under 9 months of age, pregnant women, persons with AIDS and those hypersensitive to eggs (because the vaccine contains egg white).
Information Source Links
Zoonoses - Diseases transmitted from animals to humans. Agromisia. (2008). Agrodok-Series No.46. ISBN Agromisa: 978-90-8573-105-4
